Emerging NSCLC treatments: Here are the latest drugs to keep an eye on
Last updated: 05 July 2023
You can legally access new medicines, even if they are not approved in your country.
Learn howAs lung cancer treatment research quickly advances, it can be hard to keep up with new treatment options that become available. Whether you're a new patient or you’re facing a second-line treatment, it's important to understand what is the latest in NSCLC therapy.
In this article, we'll summarize some of the new NSCLC treatments that have been approved or are in development.
Note that the goal of this summary is to create awareness of research progress, not to recommend treatments. Your doctor is best equipped to choose a treatment plan for you.
What is Non-Small Cell Lung Cancer (NSCLC)?
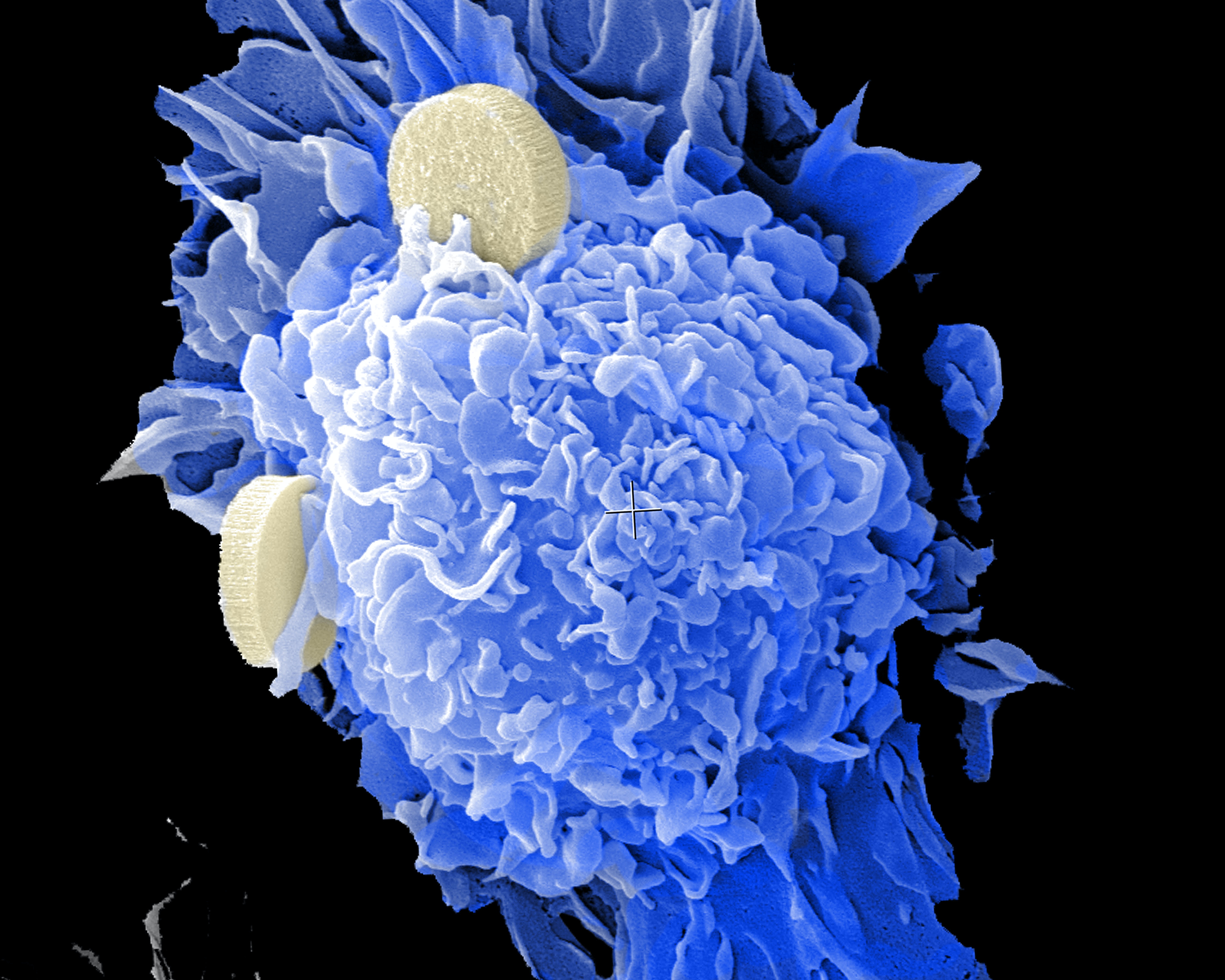
Non-small cell lung cancer (NSCLC) is a type of carcinoma - i.e. a cancer affecting the cells at the surface of the lung airways. Around 85% of all lung cancers are NSCLC, with smoking being one of the main risk factors involved.
The other main type of lung cancer is small cell lung cancer (SCLC), which is less common but more aggressive than NSCLC [1].
Types of NSCLC
Depending on which cells are affected by the cancer, NSCLC can be one of these types:
- Adenocarcinoma. This type of NSCLC usually first affects mucus-producing cells in the bronchioles, within the outer areas of the lung. Compared to other types of NSCLC, adenocarcinomas progress more slowly, which often means a better prognosis for the patient [1].
- Squamous cell carcinoma (epidermoid carcinoma). About 25-30% of NSCLC cases fall under this category. It's the one most closely associated with smoking. Squamous cell carcinoma is detected in thin flat cells across the lining of the bronchi. It tends to spread more often than other types of NSCLC, which can be a challenge for treatment [1].
- Large cell carcinoma. This type of NSCLC is rare and only occurs in 10-15% of all cases. It's an aggressive carcinoma and can be detected anywhere within the lung [1].
- Adenosquamous carcinoma. More rarely, in about 0.4-4% of NSCLC patients, this type of carcinoma is detected. It contains components of adenocarcinoma and squamous cell carcinoma [2].
- Pulmonary sarcomatoid carcinoma. The rarest and most aggressive of NSCLC types. It occurs in 0.1-0.4% of cases and has a poor prognosis [3].
What are the standard NSCLC treatments?
What treatment options are available or suitable for you depends on the stage of your NSCLC cancer, as well as your overall health.
One universal recommendation is to quit smoking. Lung cancer patients who do tend to benefit from treatment more than patients who continue smoking [4].
Apart from this recommendation, standard NSCLC treatments are:
- Surgery. If the cancer stage allows it, this is often the preferred treatment.
- Radiation therapy. Radiation targets cancer cells with high-energy rays. This kills them and prevents new ones from growing. This type of NSCLC treatment is commonly used before the tumor spreads. It can also be used as palliative care, to reduce symptoms [1].
- Chemotherapy. Chemo can be taken orally (as a pill) or as an injection. This therapy kills cancer cells and can help increase life duration with NSCLC [1].
- Immunotherapy. In short, immunotherapy drugs use different mechanisms to help the immune system fight cancer cells or to prevent cancer cells from bypassing the immune system's response [14]. This type of therapy is actively developing and is considered by many to be the future of cancer treatment.
- Targeted therapy. As its name suggests, targeted therapy focuses on specific genes and proteins that are involved in cancer cell growth and multiplication. Ideally, the therapy's 'target' is a protein present only in cancer cells. Targeted therapy is a rapidly developing area of cancer treatment. It has the potential to bring new treatment options to the table, especially for NSCLC patients with specific cancer cell mutations [15].
What are new approved treatments for non-small cell lung cancer [2023]?
Standard therapies such as chemotherapy, radiation, or surgery remain a major part of NSCLC treatment protocols. In addition to that, there is a lot of ongoing research that explores new medicines within immunotherapy and targeted therapy.
Below is a non-exhaustive list of such drugs and treatments that have already been approved for use on NSCLC patients.
Latest immunotherapy drugs for NSCLC
- Keytruda. This immune checkpoint inhibitor can be used as first-line therapy or second-line therapy of NSCLC, from stage 1 to stage 3 of the cancer. Depending on your particular situation, Keytruda can be used alone or in combination with other therapies [16].
- Imjudo (tremelimumab) in combination with Imfinzi (tremelimumab). These two drugs in combination were approved by the FDA in 2022. This therapy is applicable for NSCLC patients without changes in the ALK or EGFR gene [17].
- Opdivo (nivolumab). This previously approved immune checkpoint inhibitor is now also approved for use before surgery, in combination with platinum-based chemotherapy. A clinical trial showed that patients using this combined therapy went longer without recurrence following surgery [17].
- Libtayo (cemiplimab-rwlc). Libtayo used to be approved only as a first-line treatment for NSCLC. Now its approval extends to any stage of NSCLC, in combination with chemotherapy. Using the drug this way has shown some positive results on overall survival and progression-free survival [17].
New targeted therapy drugs for NSCLC
- Enhertu (fam-trastuzumab deruxtecan-nxki). This is the first approved drug for NSCLC with the HER2 mutation. Enhertu is a second-line treatment. It's currently approved in the USA, EU, and Japan [17].
- Krazati (adagrasib). This is the second targeted therapy drug for NSCLC with KRAS G12C mutation after Lumakras (sotorasib). There are some differences between Lumakras and Krazati, though both drugs are KRAS inhibitors and have a similar mechanism of action. Krazati is a second-line therapy, to be used after at least one previous round of systematic treatment [17]. Krazati (adagrasib) is currently only approved in the USA.
The future of NSCLC treatments: What's in development?
Cancer research is a dynamic field and new therapies are constantly in development. Below are some examples worth keeping an eye on.
Radiosensitizers
To be efficient, radiation therapy relies a lot on oxygen in cancer cells. Oxygen helps form free radicals, which damage tumor cells. However, as cancer cells grow, their blood vessels can't keep up, leaving the cells with an oxygen shortage - the so-called state of hypoxia [11]. As a result of hypoxia, radiotherapy loses its effectiveness.
Radiosensitizers aim to counteract this process. There are multiple radiosensitizers in development, but among the most relevant ones for NSCLC patients is Papaverine Hydrochloride. It will complete its Phase I Clinical trial in December 2023 [12]. The outcome of the trial will provide more clarity on the potential significance of this radiosensitizer for NSCLC patients.
Cancer vaccines for NSCLC
Another treatment avenue that may bring hope for advanced non-small cell lung cancer patients are vaccines. Over the past decade, multiple types of vaccines applicable to NSCLC have been explored.
One example is CIMAvax, which was developed in Cuba. It's currently not approved for use anywhere else. There are ongoing clinical trials with this vaccine in the USA that will deliver some more data on its efficacy by the end of 2023 [18].
Some other vaccines for NSCLC patients have shown positive safety profiles in Phase I clinical trials - e.g. the mRNA vaccine CV9201 and the neoantigen peptide-based vaccine NEO-PV-01 [13]. Further trials will clarify the potential role of these cancer vaccines in NSCLC prevention and treatment.
How to access new NSCLC treatments?
As new NSCLC drugs and therapies are developed, approval can take years in some countries. Unfortunately, this delay comes at a high price for NSCLC patients.
Is there a new NSCLC treatment not (yet) approved in your country? We can help you access it legally if you have a prescription from your doctor. Contact us to find out more.
References:
- Non-Small Cell Lung Cancer > Fact Sheets. Yale Medicine, Accessed 16 June 2023.
- Clinical characteristics and prognosis of patients with lung adenosquamous carcinoma after surgical resection: results from two institutes. Journal of Thoracic Disease, Accessed 16 June 2023.
- Pulmonary sarcomatoid carcinoma: progress, treatment and expectations. NCBI, 25 August 2020.
- Non-small Cell Lung Cancer Treatment by Stage. American Cancer Society, 27 January 2023.
- Non-Small Cell Lung Cancer: NSCLC Symptoms, Staging & Prognosis. Cancer Treatment Centers of America, 27 September 2022.
- Stage 1 Lung Cancer: Symptoms, Treatment & Survival Rate. Cancer Treatment Centers of America, Accessed 16 June 2023.
- Non-Small Cell Lung Cancer Treatment - NCI. National Cancer Institute, 16 February 2023.
- Stage 2 Lung Cancer: Signs, Symptoms, Treatment & Survival Rate. Cancer Treatment Centers of America, Accessed 16 June 2023.
- Eldridge, Lynne. Stage 3 Lung Cancer Life Expectancy. Verywell Health, 20 January 2022.
- Stage 4 Lung Cancer: Metastatic Symptoms, Treatment, Survival. Cancer Treatment Centers of America, Accessed 16 June 2023.
- The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. NCBI, 11 December 2015.
- Papaverine and Stereotactic Body Radiotherapy (SBRT) for Non Small Cell Lung Cancer (NSCLC) or Lung Metastases - Full Text View. ClinicalTrials.gov, Accessed 16 June 2023.
- Vaccine Therapy in Non-Small Cell Lung Cancer. NCBI, 9 May 2022.
- Cancer Immunotherapy > Fact Sheets. Yale Medicine, Accessed 16 June 2023.
- What is Targeted Therapy?. Cancer.Net, Accessed 16 June 2023.
- KEYTRUDA® (pembrolizumab) for Non–Small Cell Lung Cancer. Keytruda, Accessed 16 June 2023.
- Johnson, Bethany. FDA Approvals: New Treatment Landscape in 2023. GO2 for Lung Cancer, 9 February 2023.
- CIMAvax Vaccine, Nivolumab, and Pembrolizumab in Treating Patients With Advanced Non-small Cell Lung Cancer or Squamous Head and Neck Cancer - Full Text View. ClinicalTrials.gov, 4 November 2016.