Peter's story: Life goes on
Last updated: 22 July 2019
You can legally access new medicines, even if they are not approved in your country.
Learn how
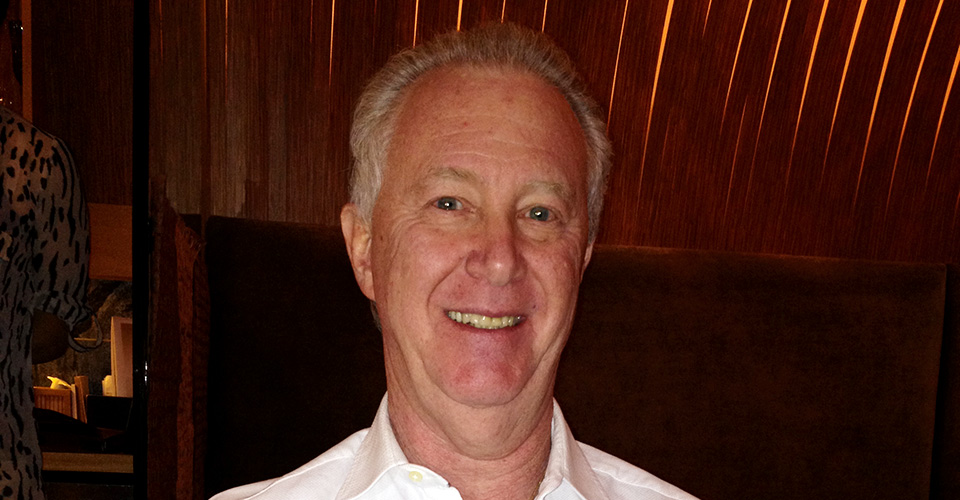
Meet Peter. He enjoys having a good work/life balance. During the week you'll find him working hard in the medical industry, but in his free time there's a high chance that you can find him on the golf green.
That was the case on a sunny day in November 2018. While taking part in a golf tournament something happened that changed his life. Peter reached for a bottle of water and realised that he was having difficulty removing the cap. Since this was a one-time occurrence, he didn't give it another moment's thought. However, on 7 January 2019, he couldn't undo the clasp of a necklace and then it hit him like a ton of bricks—something was wrong.
Diagnosis
Peter went to the hospital and got a magnetic resonance imaging (MRI) scan on his neck, brain and the left side of his heart. The scan showed stenosis, a narrowing of the blood vessels and spinal cord. After that, he was referred to a neurologist who then referred him to another neurologist who specialised in muscles. The muscle specialist ruled out problems with his neck muscles because the symptoms happened too fast. Then he was told that it could be either myeloma, neuropathy, or amyotrophic lateral sclerosis (also known as ALS, motor neurone disease (MND), or Lou Gehrig's disease).
His doctor ran four more MRIs, a computed tomography (also known as a CAT or CT scan), a positron-emission tomography (PET scan), a spinal tap and a test for 'something in the fat'. The final diagnostic was to put Peter on intravenous immunoglobulin (IVIg) to rule out infection. This immunotherapy consisted of three infusions of 1mg IVIg/kg weight over four days. Two weeks later this was followed by an outpatient procedure of three infusions of 'super doses' of 2mg IVIg/kg weight. The immunotherapy was tough and made Peter feel sick, however, it helped eliminate all the other possibilities.
The doctor then did an electromyography (EMG) to study the electrical activity of his muscles and contacted a specialised hospital. They confirmed that Peter indeed had ALS. To complicate matters, Peter found out that he also had smouldering myeloma, a pre-cancerous plasma cell disorder. Luckily, he had the less severe form so he was still eligible for ALS treatment.
The search for new ALS treatments
The deterioration of his left arm progressed rapidly, especially in the lower part, and within a month it had lost most of its function. Peter's ALS specialist was kind and intelligent but very busy. It took a long time to reach his specialist or get a response, so in the meantime Peter contacted all the doctors he knew to find out as much as he could about ALS. He looked into the known ALS medicines and found an abundance of redundant information about the top two medicines available in the USA. Next, he began researching out-of-the-box treatments and even medicines for other diseases that could also work on ALS symptoms. Finding new ALS medicines was like swimming in an endless ocean. How do you find what you don't know you're looking for?
'Once you find one [medical article or abstract on a drug] you can find a lot'.
Over time, Peter learned how to uncover the keywords that would enable him to search for new treatment possibilities. He found something on stem cell therapy, but for him it wasn't justifiable because the researchers didn't use embryonic stem cells. He also learned that medicines for Alzheimer’s and multiple sclerosis (MS) seem to work for ALS as well because the diseases follow a similar progression.
A light at the end of the tunnel
One particular medicine from Japan, ibudilast, was reported to slow the advancement of ALS. It was in phase II trials going toward FDA approval. Peter took this information to his specialist. 'Doctors are conservative', he said, and though his specialist was reluctant to speak about any non-FDA approved medicines, his specialist determined that Peter was eligible to use it and wrote him a prescription. Next, Peter had to find the medicine. Since it was only available in Japan, he contacted Japanese pharmacies who were not willing to send this medication outside of Japan, even with a prescription.
Peter went back to his specialist who referred him to our website. There he was finally able to get his medicine. 'You have been the nicest people I've dealt with', he told us. For our team, these words are priceless, because we know there is a very real struggle to access exceptional medicines, and every day we go through this struggle with the people we help.
Today
Speaking candidly, Peter said, 'The drug only works on 30 to 35% of the people and there is no way of measuring it because you don’t get better. [Now] I have less fibrillations on my arm so that might be a plus'. Currently, he takes vitamins, does acupuncture and everything recommended by his specialist to slow the ALS progression and increase his quality of life. Although the drugs and the disease make him tired, his right arm and his breathing are still strong, and he can do most things independently—including regular visits to the golf green.
'Everyone deals with these things on their own...If I was a doctor and someone came in with what I had, I would treat them for everything from Day 1.' When Peter was diagnosed, the first thing he heard was that he won't be able to walk or talk or do this or do that. 'They treat you like you are going to die. Any website can tell you that.' Instead he chooses to focus on preserving his health and continues to explore possibilities because (and I can't think of anything more fitting to end this story than Peter's own words), 'All in all, life goes on'.